|
Have you ever experienced that moment where you have some sort of deadline and you find yourself running out the door, in a mad dash, to make it on time? Noticing that both your mind and stomach are a bundle of nerves? Then all of a sudden you are forced to make an abrupt detour to the bathroom because your stomach has failed you? Or perhaps you can recall a moment when you have eaten something that has upset your body causing bloating and gas? This feeling then morphs into other ailments, creating a whole cascade of negative reactions.
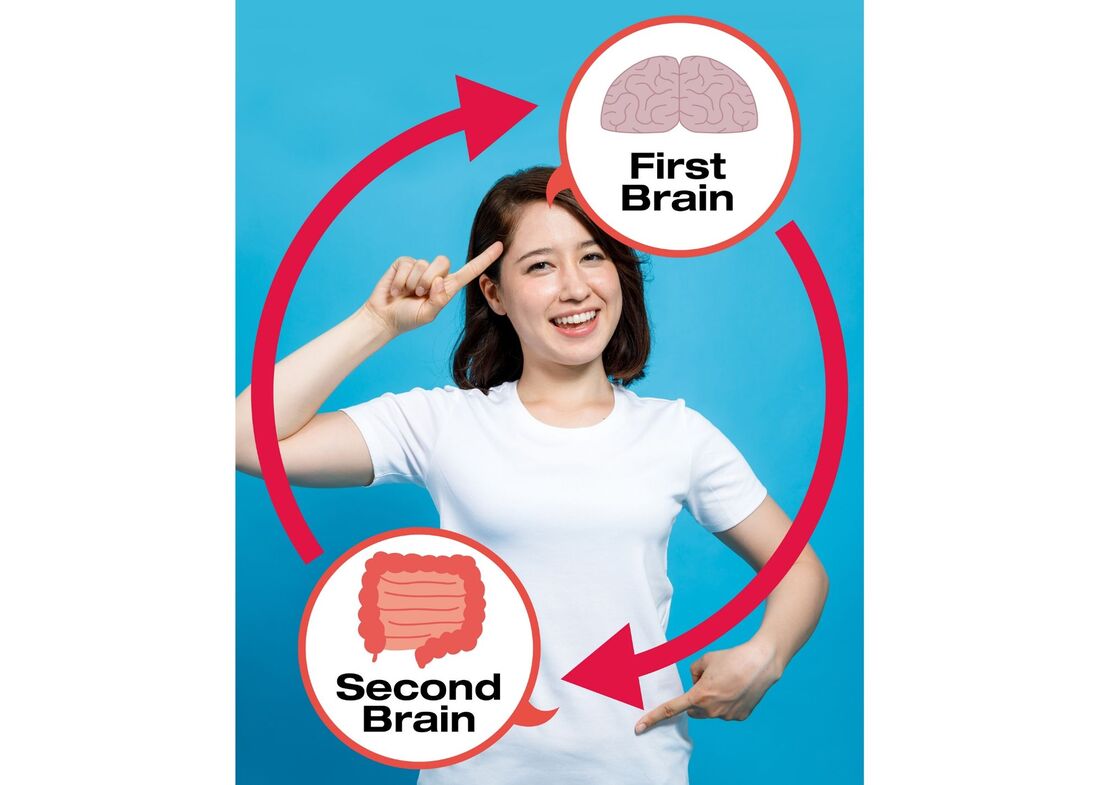
Now you observe that you have a headache and you are experiencing that brain fog where your mind feels as though it is all over the place. Perhaps you have experienced a moment where your “gut” speaks up, providing you with an intuitive feeling to avoid a specific road or to not trust a particular person? Have you stopped to ask yourself why this is happening? Well, my friend, you are not alone. The gut-brain axis is a bidirectional circuitry that runs from your central nervous system (brain and spinal cord) to your enteric nervous system (a division of the autonomic nervous system that governs the gastrointestinal tract). The gut-brain axis is a powerful mechanism that governs how you feel emotionally and physically making it our “second” brain. Let’s break it down, shall we? Our brain is constantly sending or receiving messages whether it is in response to the external environment or sensing and responding to the happenings within the internal body. Breaking it down further, what governs these feelings are the bacteria inside of the gut. What! Bacteria!? Don’t worry, I was shocked too, especially to learn that these bacteria are often the “good guys” if taken care of properly. The bacteria within our body are responsible for manufacturing nutrients, breaking down food, and when balanced helps to neutralize toxins. The gut-brain axis aids in the creation of our neurotransmitters, which are chemicals that can make us feel happy or sad. One neurotransmitter, in particular, called serotonin, regulates our mood, digestion, and appetite. Although this neurotransmitter is often known for its role in the brain, scientists are finding that the vast majority, roughly 90%, are made in the gut. With the gut holding that much power it will not be surprising to learn that about 80% of the immune system is also located in the gut. What does this mean? It means that how one chooses to fuel their body will influence the microbiome thus impacting how one feels. Food can either encourage the body to repair and heal itself by providing the right building blocks and tools, or it can be destructive adding more stress in the body further breaking it down. The HPA axis (hypothalamic-pituitary-adrenal axis) is the center for stress response. Daily, our body is combating environmental, social, financial, emotional, physical, stressors that degrade and wear down the body. The immune system is responsible for fighting pathogens and microbes (the bad guys), where the nervous system is responsible for how the body communicates. So how is it our food choices play into these systems? Well, its time to connect the dots! Once the food is ingested, the process of digestion begins, once the food particles make their way into the small intestine, it is broken down into its smallest molecular form so that it can be assimilated and used throughout the body. At this point, bacteria and the immune system are doing their jobs by protecting the body. However, if the foods that are eaten are inflammatory by nature this will result in the system going out of balance. Unfortunately, this causes the body to work overtime. If the same inflammatory foods are repeatedly eaten, it causes the HPA axis to be on high alert, in turn overburdening the immune system. This also offsets the microbiome of the gut, allowing the “bad bacteria” to dominate offsetting the good bacteria. As you can see, food choices can create a snowball effect, impacting our bacteria which influences of physical symptoms (gas, bloating) and our mental symptoms (anxiety, brain fog, depression, neurotransmitter imbalance). This can worsen diseases or disorders already present, or enhance the predisposition of a disease/ailment to “turn on.” Now that this gut-brain connection is better understood let’s discuss the foods that commonly cause inflammation. Certain foods cause the body to experience stress which causes the body to breakdown. Think of a car, if you put the incorrect gas into the vehicle repeatedly, it will cause the mechanisms to malfunction. Our body is one phenomenal mechanism that relies on us to provide full support. By avoiding specific foods, or reducing the amount of intake, you are providing the body with building blocks rather than blocks that are faulty and will eventually break. Let's take a look at some of these inflammatory foods:
This quick list compromises the most food culprits that cause inflammation. How empowering is that to know that the food you choose to ingest influences how your body feels and how your mind feels? By avoiding inflammatory foods reduces the body’s destructive stress response, it lowers the activation of the HPA axis, promotes a healthy connection between the gut and the brain, aiding the body’s resiliency to stress and disease. These foods are a means of fueling your stress rather than fueling your body. The next time you feel disconnected from yourself, overwhelmed, overly emotional, unwell physically, bloated, gaseous, take a moment to check-in. Explore if these foods could be the culprit that is fueling the break down of your body rather than the build-up. Food is power, through these choices, one can reduce the destructive stress response, enhancing their health and vitality. This guest article is written by Sky Corbett-Methot a Holistic Nutritionist and 500 hour yoga and meditation instructor. Sky is a recent graduate of the Institute of Holistic Nutrition and a previous student of both Petra Sovcov and Tahlia Sage. She is a holistic healing and wellness coach that combines a unique “just for you” approach by utilizing movement, meditation, and nourishment to enhance vitality. Find out more at about SkyYoga & Wellness at: https://www.skyyogawellness.ca Or find her on Instagram @ sky_the_dauntless References:
0 Comments
Beyond helping us extract nutrients from foods, our gut health has an important role to play in our immunity. Our gut often protests when its working conditions are less than desirable, causing heartburn, bloating, pain, gas, imperfectly-formed bowel movements. During stressful times, negative emotions can modify your gut environment in negative ways.
There are a few different ways digestive health suffers from the insult of chronic stress: Your can stress out your gut! The enteric nervous system is an extension of our autonomic nervous system, also known as the second brain. The enteric system helps to regulate digestion. When we feel stress, blood is diverted away from the digestive tract to our muscles, disrupting the intestinal muscle contraction leading to gas caused by nutrient malabsorption. Some additional symptoms like constipation and diarrhea also tend to emerge. That gut feeling is real! Stress can weaken your gut barrier. This barrier is a critical part of the immune system. A weakened intestinal barrier can let pathogens into the bloodstream leading to chronic silent inflammation that attacks our own tissues and organs, and has been linked with many chronic conditions such as Alzherarthritis, asthma, COPD, heart disease, diabetes and cancer. Inflammatory response created by our immune system is essential for protecting ourselves from infections. These inflammatory conditions take away your immune system’s resources to fend off infections. Your gut bacteria’s reaction to stress. Your gut can literally change the map in your gastrointestinal system.Your gut bacteria communicate with the brain through the vagus nerve. Your gut utilizes the same neurotransmitters your brain uses to regulate mood, memory and energy levels, such as GABA, serotonin, adrenaline, dopamine, acetylcholine and melatonin. Stress can create an immediate effect on our gut microbiome such as reduced beneficial bacteria, increased harmful bacteria and inflammation in the gut. In turn, the hostile gut environment creates defensive molecules known as inflammatory cytokines that makes the brain feel anxious and depressed. There are three foundations to good gut health: 1) Microbiome balance balance 2) Gut lining integrity 3) Sufficient digestive factors. Let’s take a look at all three factors in detail. Microbiome Balance Friendly bacteria can not only support mental emotional well-being and nutrient absorption, it can also produce natural antibiotics to kill off infections. Your gut bacteria is busy fighting off infection before pathogens can even reach your bloodstream. Adding fermented foods are a great way to reward those hard-working, good microbes. The fermentation process creates lactic acid which naturally inhibits the growth of bad bacteria. Fermented foods can also provide prebiotic fibers that help to host beneficial bacteria. However, to get the beneficial strains many of us are lacking, it’s important to introduce human strain probiotics such as any of the HMF (Human Micro Flora) line from Genestra. (We carry these at Healing House, please contact us for info) Gut Lining Integrity The gastrointestinal barrier can be reinforced by removing inflammatory food triggers to reduce the insult to the gut lining. The natural healing process can also be encouraged by adding L-glutamine, a naturally occuring amino acid found in cabbage juice and bone broth. Glutamine is the preferred fuel of the intestinal lining cells. Digestive Factors Digestive enzyme, hydrochloric acid and bile are some important digestive factors to make sure foods get broken down into nutrients. Digestive bitters such as dandelion greens, chards and arugula help to stimulate the vagus nerve, as discussed, the channel where our gut and brain communicate. Bitter herbs and foods help to aid in the production and release of digestive enzymes. Here are some recipes that support gut health: Digestive Bitters Salad Serves: 2 Total Time: 10 min Ingredients
Directions
Serves: 4 Total Time: 40 min Ingredients
Directions
Green Gut Soother Smoothie Serves: 2 Total Time: 10 min Ingredients
Directions
In health and wellness, Tahlia Sage - Holistic Nutritionist Fluids IQ is a private lab in Toronto which we use at the wellness centre. They test things such as gut permeability, inflammation, food sensitivities, candida, adrenal health, female and male hormones and so forth. Labs like this allow clients to do tests comfortably from home and mail specimens directly to the lab. With my up-coming talk at the Vancouver Health Show about raising immunity in children (February 2nd at 2pm - Vancouver convention centre), I thought that this article about the micro biome in infants was quite informative. I have copy and pasted it directly from Fluids IQ, along with the reference list. In recent years, the role that delivery method plays in the acquisition of a newborn’s gut microbiome has been an increasingly active topic1, 2. Vaginal and cesarean section deliveries have been previously shown to result in differences in the microbiome between the two in infancy, childhood and beyond.The exact role of a baby’s gut bacteria, however, is still unclear and it is not known if these differences at birth have any major effect on later health.
A new study-the largest ever of neonatal microbiomes - has been published through the ‘Baby Biome Study’3. It shows that the microbiome of vaginally delivered newborns does not come from the mother’s vaginal bacteria, as previously believed, but from the mother’s gut. This is due to the fact that during birth the newborn will come in contact with bacteria from the mother’s gut, in large part from contact with the mother fecal contents. In contrast, babies born through cesarean section have gut microbiomes that are predominantly colonized by bacteria representative of the hospital environment and more likely to have antimicrobial resistance. This recent large study used 1,679 samples of gut bacteria from nearly 600 healthy babies and 175 mothers. Fecal samples were taken from babies aged four, seven, or 21 days old, after vaginal or caesarean delivery. Some babies were also followed up later, up to one year of age.The differences in the microbiomes were largely evened out by one year old, although the authors note that large follow-up studies are needed to determine if the early differences influence later health outcomes. For the babies born via caesarean, the researchers isolated, grew, and sequenced the genomes of more than 800 potentially pathogenic bacteria, confirming that they were the same as strains causing a number of bloodstream infections. Although these bacteria don’t usually cause disease while in the gut, they can cause infections if they get into the wrong place, or if the immune system fails. In addition, most women having a cesarean are now offered antibiotics before the delivery, to help prevent the mother developing postoperative infections, meaning that the baby also receives a dose of antibiotics via the placenta. This could also cause some of the microbiome differences seen between the two birth methods. The authors of the ‘Baby Biome Study’ state that the first weeks of life are a critical window of development of the baby’s immune system, but that very little is known about it. A follow up to this study is needed, looking at these babies as they grow, to see if early differences in the microbiome lead to any health issues. This could help in understanding the role gut bacteria play in early life and could help in the development of therapeutics to create a healthy microbiome. References: 1. Dominguez-Bello, M. G. et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc. Natl Acad. Sci. USA 2010,107, 11971-11975. 2. Wampach, L. et al. Birth mode is associated with earliest strain-conferred gut microbiome functions and immune-stimulatory potential. Nat. Commun2018, 9, 5091. 3. Shao, Y. et al. Stunted microbiota and opportunistic pathogen colonization in caesarean-section birth. Nature 2019, 574, 117-121.  I am seeing more of this in clinic as of late, particularly in cases where multiple runs of antibiotics have failed and the individuals are having issues with wasting, increased GERD, and severe difficulty with nausea, slow digestion and gastric motility. When I was in school, I did quite a bit of extensive research on H-pylori and it's ties to gastrointestinal carcinomas, as it is the first confirmed carcinogenic bacterium (meaning, a bacteria that has direct ties to some gastrointestinal cancers). The following is a copy of my newest client handout, and further down you will find a copy of my research paper as well, if you are so inclined to read 45 pages of commentary about this amazing little bacterium. Helicobacter pylori is the first formally recognized bacterial carcinogen (meaning it is a bacterium that is recognized to play a part in some cancers) and is one of the most successful human pathogens, as over half of the world's population is colonized with this gram-negative bacterium. Unless treated, colonization usually persists lifelong. H. pylori infection represents a key factor in the causative factors of many gastrointestinal diseases, ranging from chronic gastritis to peptic ulcers, and some gastric cancers. It is not to say however, just because you have an h-pylori infection that there is reason to panic. This bacterium is one that both standard western medicine, and natural healers have many options available to the individual. Unlike other types of bacterium, H-pylori are adapted to live within the harsh, acidic environment of the stomach. Whereas in some cases bacterium may become eradicated by the presence of our gastric juices and hydrochloric acid within our stomach, h-pylori will instead thrive within the human GIT. It is a very opportunistic bacterium and can use specific chemical modifiers in order to penetrate the lining of the stomach where they are protected by the mucous lining in the gut. Additionally, the bacterium can interfere/communicate with the human immune system, causing it in essence to turn a ‘blind eye’ and thus it may pro-create and multiply freely within its host’s gastro-intestinal tract. Causes: Despite advances in modern medicine, the exact method of how H-pylori infections spread is generally unknown. The bacterium has existed with mankind over many thousands of years and the infections are thought to spread from oral interaction. Additionally, it may be transferred when an individual is in contact with feces. This can occur when an individual does not properly wash their hands, or if they are in contact with animal feces which interacts with mucosa such as hands going to mouth or eyes (currently theoretical). Lastly, it is believed that H-pylori can be spread via contact with contaminated food and water. It is good to know that although H. pylori has indeed been detecting in saliva, vomitus, gastric refluxate, and feces, there is currently no conclusive medical evidence for predominant transmission via any of these products. Currently the medical establishment has concluded that H. pylori is most likely contracted in childhood and from close family members who may also be silent carriers of the bacterium. In developing countries, the statistics for this are vastly different as hygiene levels and availability to clean food and water sources are often impacted. How does H-pylori impact the body? Some of the ways in which H. pylori impacts the body are the initiation of the body’s defensive inflammatory cycle, and conditions such as:
Additional diseases where H. Pylori interaction is suspected include Irritable bowel syndrome (IBS), Irritable bowel disease (IBD), Crohns, Colitis, and inflammatory diverticulosis. There is also evidence linking H. pylori to other conditions like iron-deficiency anemia and vitamin B12 deficiency. In studies there has been evidence that H. pylori has correlating factors not only with gastrointestinal diseases, but in fact it has shown correlating and contributing factors to all inflammatory disease. These include cardiovascular disease, neurological diseases, gynecological diseases, ophthalmology, skin, and oral mucosa diseases, diseases of the ears, nose, and throat, hematological diseases, hepatobiliary diseases, and issues with obesity. Symptoms and Complications of H-pylori: Most people with H. pylori infection will never have any signs or symptoms. It's not clear why this is, but some people may be born with more resistance to the harmful effects of H. pylori. When signs or symptoms do occur with H. pylori infection, they may include:
Some of the more common complications associated with H. pylori infection include:
Natural Suggestions for H-pylori Infection: Commonly Used Herbs: Echinacea - Boosts the immune system, changes the environment of the body in relation to the bacterium. This herb is a general tonic, immune modulator, immune stimulant, helps move lymph, antiseptic, anti-microbial, anti-bacterial, anti-parasitic, anti-inflammatory, detoxifier, bitter, and peripheral vasodilator. It is specific in its use for chronic infections of various types and can be used in cases of peptic ulcers, and general GIT infections. Cat’s Claw – A native to the Amazon basin, this herb is a powerful healer. Its traditional actions are: tonic, restorative, immune stimulant, antioxidant, anti-bacterial, anti-inflammatory, astringent, alterative, and can also be hypotensive. It strengthens the immune system and is a powerful agent against microbes and bacterium. Poke Root – This herb is considered a restricted herb, please see a clinical herbalist for proper dosage. For short term use, this herb is a powerful combatant against h-pylori. It is an immune-stimulant, anti-bacterial, anti-viral, anti-parasitic, anti-inflammatory, moves lymph, alterative, detoxifier, and bitter. Meadow Sweet – Often used in formulations for healing the GIT. It is astringent, antiseptic, analgesic, anti-inflammatory, antacid, carminative, digestive, liver tonic, and anti-ulcer in action. In the GIT it helps regulate gastric levels and pH. It protects and soothes the GIT mucosal lining and is specific in issues with nausea, heartburn, peptic ulcers, indigestion, diarrhea, and IBS which can be associated with H-pylori. Thyme – Common garden thyme is a very versatile herb. It is considered to be tonic, antioxidant, antiseptic, anti-microbial, anti-bacterial, anti-viral, anti-fungal, anti-parasitic, anti-inflammatory, astringent, digestive, and antispasmodic. In issues with the GIT, its astringent actions can help heal mucosal linings and it is specific in issues with gastritis and IBS. Plantain Leaf – Traditionally used in cases where mucosal membranes need healing. Plantain leaf is antiseptic, anti-microbial, anti-bacterial, anti-inflammatory, demulcent, refrigerant, alterative, blood tonic, and antacid in action. In the GIT it is a soothing agent and is often used specifically in issue with acidity and gastritis. Oregon Grape Root – This herb is rich in berberine and is tonic, antiseptic, anti-microbial, alterative, hepatic, and anti-bacterial. It is specific as a general blood cleanser with its actions upon the liver, and can be used for conditions of the GIT. Commonly Used Supplements: Multi-Vitamin – For the general function of all metabolic and cellular functions. This is an aggressive bacterium; the body needs every opportunity to heal. CoQ10 – Improves cellular oxygenation, protects cardiovascular health, and promotes proper circulation. Vitamin B Complex – Needed for proper digestion, metabolic function, and cellular repair from inflammation. Potassium – Increases cellular metabolism and aids in balancing blood pH. Vitamin A – Helps to protect the mucous membranes and to protect the body from the damages of the inflammatory cycle. Colostrum – Promotes accelerated healing of the GIT and boosts the immune system. Probiotic – Supports the re-establishment of gut health, improves healing and lowers inflammation. Dietary/Lifestyle Suggestions:
References:
|
Petra Sovcov is not a Medical Doctor (MD) nor a Naturopath (ND), she is a Clinical Herbal Therapist (CHT) and holds a Doctorate in Natural Medicine (DNM). The suggestions or recommendations made on this site are not meant to be a substitute for advice from your MD, or as a substitute for any prescriptions you may be taking. Suggestions followed will be the responsibility of the reader, and are stated with the intention of interest and education only. If you have a health issue, please see your primary care physician (MD) first and foremost. Categories
All
Archives
July 2024
|



 RSS Feed
RSS Feed